
#First lipid emulsion therapy used serial
Serial ECGs looking for evidence of sodium channel blockade (prolonged PR and QRS intervals, large terminal R wave in aVR) Management UEC, arterial blood gas, methaemoglobin concentration Methaemoglobinaemia: blue mucous membranes progressing to CNS and cardiovascular manifestations of cellular hypoxia and then death.Ĭardiac arrest may be the first clinical manifestation following massive intravenous overdose.Īlways check for Medicalert bracelet in any unconscious patient, or any other signs of underlying medical condition (fingerprick marks etc) Investigations.Respiratory: respiratory depression, apnoea.Cardiovascular: bradycardia, hypotension, atrial and ventricular dysrhythmias, conduction blocks, cardiovascular collapse, asystole.Anxiety, agitation, confusion, disorientation, drowsiness.Larger doses can safely be given with adrenaline.īupivocaine is particularly cardiotoxic. Please note that toxicity can still occur with doses lower than these when given via intravenous or intra-arterial injection. The following table outlines the maximum recommended doses for various local anaesthetic agents. Calculate the maximum possible dose per kg.Any patient whose developmental age is inconsistent with accidental poisoning as non-accidental poisoning should be considered.All patients with deliberate self-poisoning (uncommon) or significant accidental overdose or inadvertent venous or arterial injection.Most agents have elimination half-lives of 2 hours, but bupivacaine has a longer elimination half-life (5 hours or longer). Most local anaesthetics are eliminated by hepatic metabolism. The presence or not of adrenaline in the preparation.This in turn depends on a number of factors, including There may be other effects, including blockade of potassium and calcium channels, interaction with cholinergic or N-methyl-D-aspartate (NMDA) receptors and interference with cellular metabolic processes.Ĭlinical manifestations correspond to the concentration in the systemic circulation. The toxic mechanism is via local anaesthetic agent binding reversibly to sodium channels. Although there is extensive first-pass metabolism, there are reported fatalities following the ingestion of lignocaine-containing local and topical preparations. Situations leading to toxicity include inadvertent venous or arterial injection as well as too high a dose of ingested or topically administered local anaesthetic-containing preparations. Local anaesthetic toxicity generally occurs as a result of therapeutic error. Allergic reactions including anaphylaxis are also possible and should be treated along conventional lines - see Anaphylaxis.įor 24 hour advice, contact Victorian Poisons Information Centre 13 11 26 Background.It is not dose-related and is more likely to occur in children, including following topical administration.

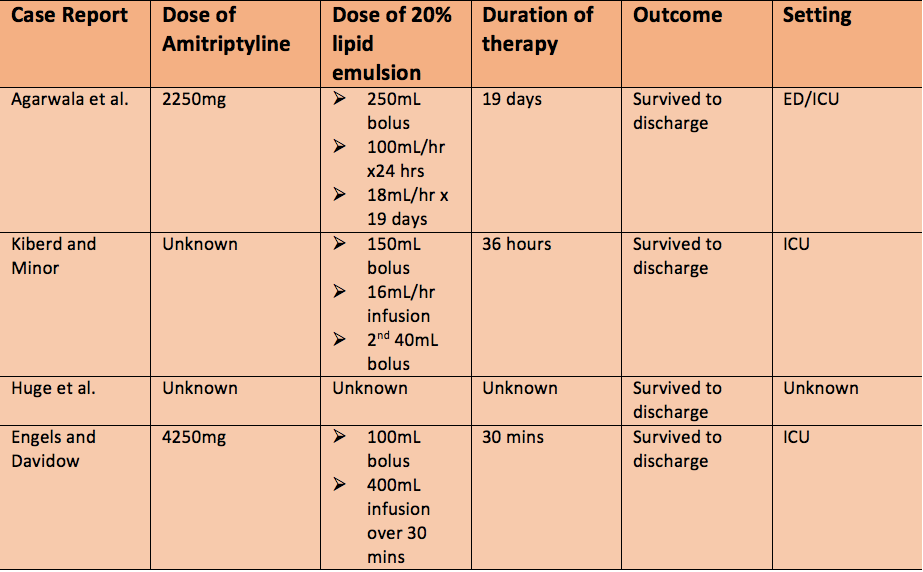
Management of local anaesthetic toxicity is largely supportive, with the use of intravenous lipid emulsion in severe cases.However symptoms and signs of toxicity can occur after a longer period of time following oral or topical administration. Onset of local anaesthetic toxicity is usually rapid, with serious and potentially fatal neurological and cardiovascular manifestations.Poisoning – Acute Guidelines for Initial Management Anaphylaxis Resuscitation Key points


 0 kommentar(er)
0 kommentar(er)
